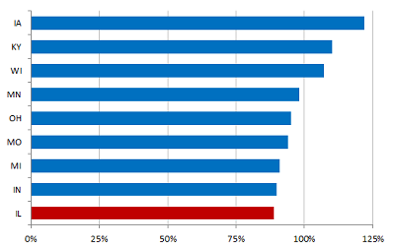
* The Illinois Policy Institute took a look at Medicaid reimbursement rates to health care providers and found that Illinois has the lowest…
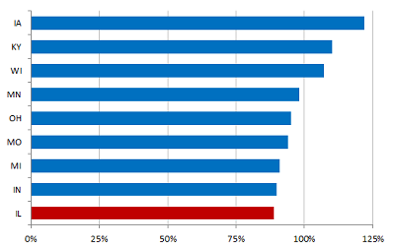
* From the Institute…
Illinois already has the lowest reimbursement rate in the region. In many cases, they don’t even cover the actual cost to provide services.
The program reimburses doctors so poorly that many simply cannot afford to take more Medicaid patients. This leaves most Medicaid patients competing with each other for fewer and fewer doctors willing to see them. In Chicago, for example, children with throat cancer have only a one-in-three chance of seeing a specialist if they’re enrolled in Medicaid. For those with juvenile diabetes or epilepsy, the odds of seeing a specialist are one-in-two. And even when they can get an appointment, they have to wait months just to see the doctor. Cutting those rates even further doesn’t solve the problem. It just leaves the poorest and most vulnerable with even fewer options to receive quality care.
* The Illinois Hospital Association’s reaction to Gov. Pat Quinn’s Medicaid proposal yesterday is worth reading in full…
The Illinois Hospital Association (IHA) and the hospital community are deeply concerned about the Governor’s Medicaid proposal calling for a major rate cut to hospitals of about $350 million or approximately 8 percent. This proposed rate cut is in addition to about $150 million in other proposed reductions directly targeted at hospitals.
While we commend the Governor for taking some positive steps – including incorporating several of IHA’s savings alternatives – the proposal is still too drastic and too rash to impose on the state’s already fragile health care system. Simply engaging in a math exercise to fill a budget gap is the wrong approach that will hurt patients.
A reduction of this magnitude will jeopardize patients’ access to quality health care, cause irreparable harm to the Medicaid program and the health care system, and undermine hospitals in their critical roles as health care providers and major job creators. About one-third of Illinois hospitals are now losing money, and Illinois currently ranks 44th in the U.S. in per beneficiary Medicaid spending. Under the Governor’s proposed rate cut, many hospitals will be forced to reduce or eliminate key services or lay off staff – or both – and some hospitals may close.
The hospital community recognizes that the state’s budget challenges are significant. We want to partner with the Governor and the General Assembly on workable solutions that will help address those challenges. To that end, IHA and the hospital community have offered a series of alternatives to generate substantial cost savings and new revenues for the Medicaid program, totaling as much as $1.4 billion. (See IHA’s alternatives at: http://tinyurl.com/6t8doaw)
We urge the General Assembly to consider several alternatives that are either excluded from or undervalued in the Governor’s proposal in order to avoid blunt rate cuts, including:
· Maximizing revenues – both federal and other revenues – including enhancing the Hospital Assessment Program;
· Improving verification of eligibility for new and current beneficiaries; and
· Increasing provider based care coordination by enhancing the current Primary Care Case Management Program (which has saved the Medicaid program than $400 million since 2007).
IHA and the hospital community are firmly committed to working with the General Assembly on meaningful solutions – in a multi-year approach – to address the state’s budget challenges while transforming the Medicaid program to be sustainable and cost effective for the people of Illinois.
* Statement from Health Care Council of Illinois Executive Director Pat Comstock…
Our initial review of the governor’s proposal suggests there is a $237 million cut for nursing homes, an enormous amount. Such a cut would be devastating for resident care at nursing homes throughout the state. If that dollar amount proves to be accurate, it would decimate the money we generated by taxing ourselves to pay for recent safety reforms.
Discuss.















- just sayin' - Friday, Apr 20, 12 @ 11:28 am:
Old people all just need to get 6 figure jobs in a “non-profit” and a PAC like IPI’s John Tillman where they can get paid to bemoan the pensions that government workers who make 30 or 40 grand get. Problem solved.
- so.... - Friday, Apr 20, 12 @ 11:34 am:
Well I guess that’s one way to reduce Medicaid outlays. You reduce payments to providers by so much that no one will accept Medicaid patients. If no Medicaid recipients can get treatment, then no Medicaid money gets spent. Problem solved!
P.S. - Just as an aside, I really wish people would stop improperly using the word “decimate”. When you decimate something, you reduce it by 1/10th. It’s not just a $10 word alternative to “destroy”.
- Beef_Eater - Friday, Apr 20, 12 @ 11:39 am:
My wife is a dentist. Adult Medicaid pays about $13 for a filling. To really do the filling correctly, it costs $16 in material(composite). This is why she doesn’t usually take adult medicaid already. It is proposed to get rid of adult dental care. This would actually be good because a lot of the people truly can afford it on their own but don’t want to pay as they have medicaid. All kids is a different story. It pays a little better and it is harder to turn down children.
- Been There - Friday, Apr 20, 12 @ 11:46 am:
===Our initial review of the governor’s proposal suggests there is a $237 million cut for nursing homes, an enormous amount.====
$237 mil is an enormous amount and it works out to $2370 per nursing home patient if there are 100,000 people in nursing homes as estimated. Now of course not all of them are on Medicare so the per person amount goes up for just those on the program. On the other hand for what they charge the non-medicare patients my guess is this will be around 5-6% of their income. Pretty close to what the state is asking others to take a cut.
- Cook County Commoner - Friday, Apr 20, 12 @ 11:57 am:
Won’t a reimbursement rate cut just result in increased charges to non-Medicaid patients by those health care providers that stay in Illinois? And doessn’t that mean increased payouts for governemt retiree healthcare benefits? So the private sector workers gets slammed twice: once at doctor’s office and then again on increased taxes to feed the governement retirees’ health care system. It just keeps getting worse.
- dave - Friday, Apr 20, 12 @ 12:36 pm:
I find it fascinating that IPI appears to be coming out against rate cuts.
So it is small government and less government spending in terms of services/eligibility, but providers? Nah… they don’t need a rate cut.
- dave - Friday, Apr 20, 12 @ 12:38 pm:
**Won’t a reimbursement rate cut just result in increased charges to non-Medicaid patients by those health care providers that stay in Illinois?**
I thought you conservatives believed that the market drove everything.
Private-pay rates have little/nothing to do with the state’s Medicaid rates. Private-pay rates (as paid by insurance) are largely the result of how low the big insurance companies have drive rates down (while making billions in profits).
- Elder - Friday, Apr 20, 12 @ 12:57 pm:
It is unseemly for the hospitals to be poor mouthing while some of these “nonprofits” sit on literally billions of dollars in “reserves” (profits) and they resist calls for charity care.
- kerfuffle - Friday, Apr 20, 12 @ 1:10 pm:
=== some of these “nonprofits” sit on literally billions of dollars in “reserves” (profits) and they resist calls for charity care==
Really - billions of dollars!
- OneMan - Friday, Apr 20, 12 @ 1:16 pm:
For those folks paying retail, yes it may result in higher costs, however since most reimbursement is set by the insurance companies. So the answer for a medical practice is going to be to see fewer medicade patients.
- Capital View - Friday, Apr 20, 12 @ 1:43 pm:
As I just advised Sara Feigenholtz, the best approach is to have each of the health and human services agencies rank their community based providers by performance indicators, and then eliminate Medicaid eligibility and state funding to the bottom 10 or 15% of providers. Don’t clobber the well functioning agencies, but use this fiscal crisis to dump the worst performing.
Give a tiny rate increase to the highest performing agencies in terms of effectiveness, as well.
IDPA Director Greg Coler culled the number of hospitals this way back in the early 1980s. He used the device of rate negotiations, offered totally dysfunctional rates to certain deficient hospitals so that they chose to close their doors, not that the state forced them to do so. Nonsense - do the honorable thing and declare losers as of the beginning of next fiscal year based on performance indicators.
- dave - Friday, Apr 20, 12 @ 2:01 pm:
**Really - billions of dollars! **
Maybe not billions… but Northwestern, one of the key figures in the charity care fight, is sitting on over a full year of cash on hand.
Some of the real safety-net hospitals, on the hand, literally have less than 5 days of cash on hand.
- dave - Friday, Apr 20, 12 @ 2:02 pm:
**the best approach is to have each of the health and human services agencies rank their community based providers by performance indicators, and then eliminate Medicaid eligibility and state funding to the bottom 10 or 15% of providers. **
Yet you still have the same number of enrollees, and you want higher rates, so how does this address the fiscal problems?