It’s just a bill
Tuesday, Sep 17, 2019 - Posted by Rich Miller
* Press release…
State Senator Andy Manar (D-Bunker Hill) gathered with fellow state lawmakers and diabetes health advocates in Springfield Tuesday to urge support for new a new measure aimed at reducing the skyrocketing price of insulin.
“There are people in this state who have to choose between buying their prescription insulin and paying for groceries or making their mortgage payment,” Manar said. “These prices are absolutely out of control and we have a responsibility as lawmakers to take immediate action to ensure that every person has access to the care they need.”
Senate Bill 667, introduced by Manar, would cap out of pocket insulin expenses at $100 for a 30-day supply.
Manar was joined by State Rep. Sue Scherer (D-Decatur) to push for the legislation’s passage and hear from individuals who have been directly impacted by rising insulin costs.
“It’s been 10 years since the insulin I need to survive was only $800. Now it cost $1800,” said Megan Blair, a single mother who has experienced firsthand the consequences of rising insulin costs. “Something needs to change. Something has to be done about this.”
According to the American Diabetes Association, there are over 30 million Americans who have diabetes, 7.4 million of which require prescription insulin every day to survive. However, the increasing costs associated with the medication have led many patients to ration their supply or seek care outside of the country.
The legislation would make Illinois just the second state in the country to cap out of pocket insulin expenses. Colorado became the first to do so earlier this year.
“We cannot continue to sit back and allow drug companies to charge exorbitant prices on lifesaving medication that people depend on every day,” said Rep. Will Guzzardi, the bill’s lead sponsor in the House. “Instead of crushing Illinois consumers to pad corporate profits, let’s take real action to prioritize the actual health and well-being of Illinois residents who rely on insulin.”
The legislation has also garnered the support of several advocacy organizations, including the American Diabetes Association, Illinois State Medical Society, Illinois Pharmacists Association and AARP.
“AARP Illinois supports this measure on behalf of our 1.7 million members, many of whom have told us about the hardships they face in paying for their prescription drugs,” said State Director Bob Gallow. “We commend Sen. Manar, Rep. Guzzardi, and other legislators for recognizing that everyday Illinois residents are having to make heartbreaking choices about whether to pay for medicine or other basic necessities with their fixed incomes. And we hope that SB 667 will be a stepping stone to getting further reforms that will lower the cost of prescription drugs for everyone.”
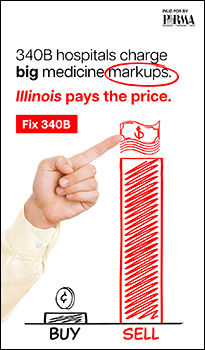
Opponents include the Illinois Chamber of Commerce, the Illinois Retail Merchants Association, the Illinois Manufacturers’ Association, BlueCross BlueShield of Illinois, Eli Lilly and Company, the Illinois Insurance Association, the Pharmaceutical Research and Manufacturers of America and others.
* More from AARP…
* Peoria Public Radio…
Manar was joined by state Sen. Dave Koehler (D-Peoria), state Rep. Jehan Gordon-Booth (D-Peoria), two people with diabetes, and local health care professionals. Gordon-Booth said it’s important to remember African-Americans are twice as likely to deal with diabetes than non-Hispanic whites.
“If we’re talking about ensuring the ability of people to live safe and healthy lives, they have to have access to insulin. It’s not optional. It’s mandatory,” she said.
She said several members of her family have struggled with this issue, and mentioned she struggles with high blood pressure despite maintaining a healthy diet and lifestyle.
* Journal Star…
Because she struggles to pay for insulin, Megan Blair has been hospitalized multiple times in the 10 years since she was diagnosed with Type 1 diabetes at the age of 18. […]
“It turned into a game for me. How much insulin could get me through the day? If I don’t give myself all the insulin I need in one day, I would have leftovers for the next day and maybe I could learn how to turn this 30-day supply into a 60-day supply,” she said. “Well, this worked for a little bit, until my body couldn’t keep functioning … I ended up in the hospital several times.” […]
“The total cost of care of patients with diabetes goes up when you don’t take care of diabetes, making them at increased risk for heart attacks and strokes. Who pays for that? Everybody who pays taxes pays for that, and everyone that has private insurance pays for that through increased insurance costs,” said [Dr. Gregg Stoner, the medical director for the Heartland Clinic]. “So while patients suffer from the physical consequences of diabetes, we all share in the cost.” […]
“In Colorado, where they have already passed a similar bill, it has not raised any costs of insurance on anybody else,” said Koehler. “If you think about it, making sure people have insulin when they need it probably prevents a lot of ER visits, and a lot of other medical costs that could have been avoided.”
…Adding… International context…















- Da Big Bad Wolf - Tuesday, Sep 17, 19 @ 12:56 pm:
Wait a minute, Blue Cross Blue Shield wants to pay MORE for diabetics to go to the ER?
- RNUG - Tuesday, Sep 17, 19 @ 1:05 pm:
While I normally prefer less regulation than more, drug cost / profiteering has gotten to the point where the government should intervene in the market. For long established drugs (and their variants intended to just extend patent protection), government might want to consider limiting said drugs retail cost to something like 3 or 4 times audited and verified production cost.
It’s not like it is a new drug that has to recover R&D costs. And for lifesaving drugs, where is the need to advertise? Everybody who needs to already knows about the drug.
- Anon221 - Tuesday, Sep 17, 19 @ 1:26 pm:
Will this apply to patients in hospitals and/or nursing homes? There is still a lot of sliding scale injections of insulin done in many long-term and nursing homes. Will there be a $100 cap for those patients as well- honest question.
Related- https://khn.org/news/millions-of-diabetes-patients-are-missing-out-on-medicares-nutrition-help/
- Dan Johnson - Tuesday, Sep 17, 19 @ 1:33 pm:
I’m a broken record but most employers would love this bill. Paying less for drugs would be great. It’s frustrating that the voices of employers are always siding with the largest for-profit companies instead of the hundreds of thousands of employers who would be better off if this bill were law. Not to mention the greater purchasing power of patients to spend their money in Illinois shops instead of insulin.
THis
- Smalls - Tuesday, Sep 17, 19 @ 1:37 pm:
Imagine a drug company could charge you for the air you breathe. And they know you would die without it, so they can charge you whatever they want and you have no choice but to pay it. This is exactly what life as a Type 1 diabetic is like. They will literally die within days without insulin. Fix the broken system.
- Rasselas - Tuesday, Sep 17, 19 @ 1:54 pm:
If I understand this bill, it doesn’t limit what drug companies can charge, it limits what patients can be charged as co-pays by their insurer. That means that the cost isn’t being limited, just shifted. Drug companies don’t lose, insurers and employers do. And we all pay, directly or indirectly, the cost of insurance or employer’s cost.
What we really need is something to lower the cost of drugs. Since Illinois legislators don’t really have the power to do this, they instead choose to make it look like they’re doing something by doing this. But it’s just cost shifting, not cost saving.
- Rich Miller - Tuesday, Sep 17, 19 @ 1:59 pm:
===But it’s just cost shifting, not cost saving===
Isn’t putting the squeeze on drug-makers also cost-shifting?
- Rasselas - Tuesday, Sep 17, 19 @ 2:52 pm:
I just re-read the bill. It only affects the co-pays insurers may require from patients. It doesn’t affect what drug companies can charge pharmacies and hospitals (who are then reimbursed by the insurers). (And, of course, it doesn’t affect people who are uninsured, or who get their coverage through ERISA plans at work, who are nearly half the insured population). So I don’t see how that squeezes drug-makers. Am I missing something?
- JackD - Tuesday, Sep 17, 19 @ 7:56 pm:
If the drug companies keep this up, they’ll get socialized medicine a lot quicker.